
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Original Articles
- Cardiovascular Risk/Epidemiology
- Two-Year Changes in Diabetic Kidney Disease Phenotype and the Risk of Heart Failure: A Nationwide Population-Based Study in Korea
- Seung Eun Lee, Juhwan Yoo, Han Seok Choi, Kyungdo Han, Kyoung-Ah Kim
- Diabetes Metab J. 2023;47(4):523-534. Published online April 25, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0096
- 1,718 View
- 100 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
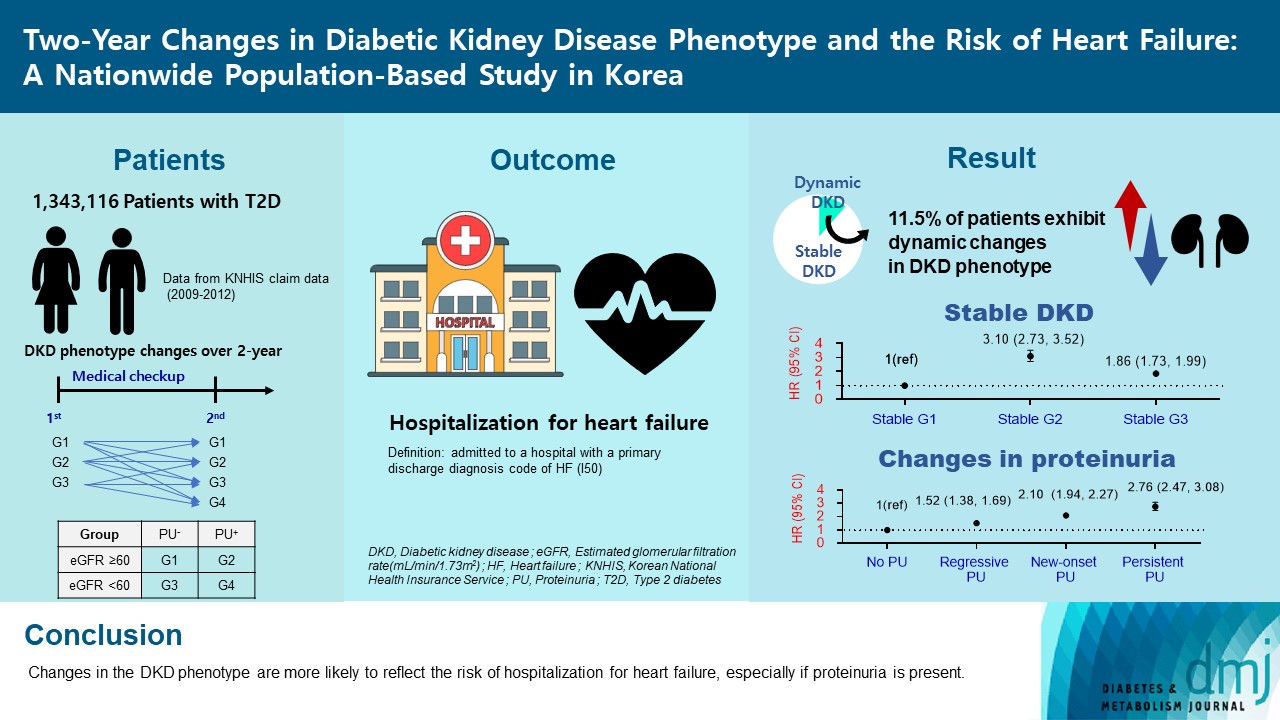
Diabetic kidney disease (DKD) is a risk factor for hospitalization for heart failure (HHF). DKD could be classified into four phenotypes by estimated glomerular filtration rate (eGFR, normal vs. low) and proteinuria (PU, negative vs. positive). Also, the phenotype often changes dynamically. This study examined HHF risk according to the DKD phenotype changes across 2-year assessments.
Methods
The study included 1,343,116 patients with type 2 diabetes mellitus (T2DM) from the Korean National Health Insurance Service database after excluding a very high-risk phenotype (eGFR <30 mL/min/1.73 m2) at baseline, who underwent two cycles of medical checkups between 2009 and 2014. From the baseline and 2-year eGFR and PU results, participants were divided into 10 DKD phenotypic change categories.
Results
During an average of 6.5 years of follow-up, 7,874 subjects developed HHF. The cumulative incidence of HHF from index date was highest in the eGFRlowPU– phenotype, followed by eGFRnorPU+ and eGFRnorPU–. Changes in DKD phenotype differently affect HHF risk. When the persistent eGFRnorPU– category was the reference, hazard ratios for HHF were 3.10 (95% confidence interval [CI], 2.73 to 3.52) in persistent eGFRnorPU+ and 1.86 (95% CI, 1.73 to 1.99) in persistent eGFRlowPU–. Among altered phenotypes, the category converted to eGFRlowPU+ showed the highest risk. In the normal eGFR category at the second examination, those who converted from PU– to PU+ showed a higher risk of HHF than those who converted from PU+ to PU–.
Conclusion
Changes in DKD phenotype, particularly with the presence of PU, are more likely to reflect the risk of HHF, compared with DKD phenotype based on a single time point in patients with T2DM.
- Cardiovascular Risk/Epidemiology
- Comparative Effects of Sodium-Glucose Cotransporter 2 Inhibitor and Thiazolidinedione Treatment on Risk of Stroke among Patients with Type 2 Diabetes Mellitus
- Seung Eun Lee, Hyewon Nam, Han Seok Choi, Hoseob Kim, Dae-Sung Kyoung, Kyoung-Ah Kim
- Diabetes Metab J. 2022;46(4):567-577. Published online February 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0160

- 5,434 View
- 358 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Although cardiovascular outcome trials using sodium-glucose cotransporter-2 inhibitors (SGLT-2i) showed a reduction in risk of 3-point major adverse cardiovascular events (MACE), they did not demonstrate beneficial effects on stroke risk. Additionally, meta-analysis showed SGLT-2i potentially had an adverse effect on stroke risk. Contrarily, pioglitazone, a type of thiazolidinedione (TZD), has been shown to reduce recurrent stroke risk. Thus, we aimed to compare the effect of SGLT-2i and TZD on the risk of stroke in type 2 diabetes mellitus (T2DM) patients.
Methods
Using the Korean National Health Insurance Service data, we compared a 1:1 propensity score-matched cohort of patients who used SGLT-2i or TZD from January 2014 to December 2018. The primary outcome was stroke. The secondary outcomes were myocardial infarction (MI), cardiovascular death, 3-point MACE, and heart failure (HF).
Results
After propensity-matching, each group included 56,794 patients. Baseline characteristics were well balanced. During the follow-up, 862 patients were newly hospitalized for stroke. The incidence rate of stroke was 4.11 and 4.22 per 1,000 person-years for the TZD and SGLT-2i groups respectively. The hazard ratio (HR) of stroke was 1.054 (95% confidence interval [CI], 0.904 to 1.229) in the SGLT-2i group compared to the TZD group. There was no difference in the risk of MI, cardiovascular death, 3-point MACE between groups. Hospitalization for HF was significantly decreased in SGLT-2i-treated patients (HR, 0.645; 95% CI, 0.466 to 0.893). Results were consistent regardless of prior cardiovascular disease.
Conclusion
In this real-world data, the risk of stroke was comparable in T2DM patients treated with SGLT-2i or TZD. -
Citations
Citations to this article as recorded by- Similar incidence of stroke with SGLT2 inhibitors and GLP-1 receptor agonists in real-world cohort studies among patients with type 2 diabetes
André J. Scheen
Diabetes Epidemiology and Management.2024; 13: 100179. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Do SGLT2 inhibitors and GLP-1 receptor agonists modulate differently the risk of stroke ? Discordance between randomised controlled trials and observational studies
André J. Scheen
Diabetes & Metabolism.2023; 49(5): 101474. CrossRef
- Similar incidence of stroke with SGLT2 inhibitors and GLP-1 receptor agonists in real-world cohort studies among patients with type 2 diabetes
- Efficacy of Serum Leptin Level as an Indicator to Predict the Clinical Response of Rosiglitazone in Patients with Type 2 Diabetes Mellitus.
- Jae Hyuk Lee, Soo Kyung Kim, Kyu Yeon Hur, Han Seok Choi, Ji Young Jung, Wan Sub Shim, Hyun Joo Lee, Chul Woo Ahn, Sung Kil Lim, Kyung Rae Kim, Hyun Chul Lee, Bong Soo Cha
- Korean Diabetes J. 2003;27(5):420-432. Published online October 1, 2003
- 1,323 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Leptin is a protein secreted by adipocytes that regulates food intake by acting on the hypothalamus and is correlated with body fat mass. Insulin resistance is also correlated with body fat mass and obesity. Rosiglitazone (RSG) is known as a highly selective and potent agonist for the peroxisome proliferator-activated receptor-gamma (PPARgamma). It improves glycemic control by improving insulin sensitivity in peripheral tissue. This study was performed to evaluate the antidiabetic and insulin sensitizing effects of RSG combination therapy and the efficacy of serum leptin level as an indicator to predict the clinical response of RSG in type 2 diabetic patients with oral agents such as metformin and/or sulfonylurea. METHODS: The study subjects were 140 type 2 diabetic patients (90 male, 50 female) who received a 12-week course of daily 4 mg RSG, in addition to the previous medications. The glucose level, indices of insulin resistance and metabolic parameters were measured. Serum leptin level was measured by radioimmunoassay before and after RSG treatment. Visceral fat and subcutaneous fat were measured by sonography. RESULTS: After 12 weeks of RSG treatment, FPG (12.6+/-28.1 mg/dL), HOMAIR (0.3+/-0.9), serum fasting insulin (1.9+/-4.7 microU/mL), SBP and DBP had all decreased significantly, whereas body weight, BMI, waist circumference, WHR, body fat mass, and subcutaneous fat had all increased. Serum leptin level also tended to increase after RSG treatment, but without significance. deltaFPG (delta=value after treatment- value before treatent) was inversely correlated with basal serum leptin level (r=-0.202), basal HOMAIR (r=-0.226) and basal FPG (r=-0.565). There was no correlation between deltaFPG and basal BMI or serum insulin level. RSG treatment showed significant inverse correlation between serum leptin level and deltaHOMAIR (r=-0.416), delta insulin (r=-0.365) and deltaHbA1c (r=-0.189). Serum leptin level was positively correlated with the subcutaneous fat amount (r=0.548), basal BMI (r=0.521), and basal HOMAIR (r=0.343). CONCLUSION: These results showed that RSG treatment can improve not only hyperglycemia but also insulin resistance in type 2 diabetic patients. The serum leptin level at baseline can be used as an indicator to predict the clinical response of RSG treatment in type 2 diabetes patients.

 KDA
KDA
 First
First Prev
Prev





